Accepting New Patients
Functional Medicine for Chronic Foot and Ankle Pain
Functional Medicine for Chronic Foot and Ankle Pain

Chronic foot pain is not an uncommon malady. It has become more and more prevalent amongst the foot suffering population. Many of these patients have sought professional care and have received anti-inflammatory therapies (cortisone injections or prescription oral anti-inflammatory medications), physical therapy, orthotics and surgical procedures. Yet, in spite of all of this, there is a growing number of patients who “do not respond” to these traditional therapeutic approaches. Many are labeled “difficult patients who can’t be pleased” and others just seem to fall through the cracks of our current medical system.
Is it the therapies that are faulty? Afterall, these traditional approaches do help the majority of patients. It is not fair to condemn the therapies themselves. The fault lies in the lack of trying to ascertain why these patients do not respond to these oft successful procedures. In other words, we need to know not only what the diagnosis is (to be certain there was not a misdiagnosis), but also to understand each one of these patients’ unique epigenetics, genetics and the current health of their immune system to uncover the reasons why they are struggling to heal.
This approach to understanding each patient’s unique physiology and how it intertwines with their total health and the ability of the immune system to maintain homeostasis is called functional medicine. Patients experiencing chronic pain have a reason for the pain syndrome and a reason why they have not responded to conventional therapies. Let’s look at a hypothetical case loosely based on a patient of mine so it becomes clear and easier to understand.
Our patient, a 52 year old female, presented to her original primary care doctor with heel pain that had been present for three months and did not seem to be showing any signs of letting up. She was referred to a podiatrist who took an x-ray and diagnosed her with a heel spur. He administered a cortisone injection, prescribed an oral, non-steroidal anti-inflammatory medication and told her to stretch her calf 3 times daily. She was told to return in two weeks. Upon her return to the doctor, she reported a 75% decrease in the pain intensity and frequency. She received another cortisone injection and was told to continue the oral medication and the calf stretches. She was told to return to the office in two weeks. After experiencing no pain for a week (even after taking long walks), she canceled her follow up appointment and stopped taking the medication.
One week after discontinuing the medication, her pain returned, only it felt more intense than it had originally. Frustrated, she went to see the podiatrist again, who assured her that she simply stopped taking the medication too soon. He renewed her prescription and also gave her a third cortisone injection. She was told to return in a month. When she returned, she again reported feeling better but there was not 100% improvement. The doctor told her she needed orthotics and that would solve the problem. She was casted for the orthotics and was told they would be in the office in approximately 3 weeks. During that time, she continued stretching her calf and taking the medication.
She returned to the podiatrist to have the orthotics dispensed. She reported some good days and many more bad days in spite of the medication. Some days she reported her pain as low as 3/10 and some days 7-8/10. To sum up her situation thus far, she had received 3 cortisone injections in her heel, was taking oral medication for 6 weeks and was stretching her calf every day. The doctor told her to break the orthotics in slowly over the course of a week and to return if there were any issues. No treatment was rendered. She was just told to stay on the medication.
She returned one week later with a report that the orthotics made her pain much worse and she wasn’t able to wear them more than 3 hours a day. The doctor now seemed visibly annoyed with her and told her that he will adjust the orthotic. He came back into the treatment room, handed her the orthotics and told her to try them for two more weeks.
She returned to the office in two weeks, still asserting that the orthotics make her pain worse and she can’t wear them. She had now been on the prescription medicine for 9 weeks. Her pain levels persisted as before. The doctor gave her another cortisone shot and gave her a prescription for physical therapy. He told her to return for a follow up appointment in two months.
One month into physical therapy, she began feeling sick in her stomach every day. After 4 days of not feeling well, she went to her internist. After his exam, he suspected that the oral medication “wasn’t agreeing with her” and told her to stop taking it. He also did some blood work which came back two days later with elevated liver enzymes. Her internist told her it was from the medication but it should return to normal if she doesn’t take it. After discontinuing the medication, her stomach issues persisted and the heel pain was much worse again.
In frustration, she decided to get a second opinion and called my office. After she related the prior 6 month history of her problem and all related treatments, I started my consult with a review of systems. This means we ask questions about every part of her body to find out if there are any obvious struggles in her physiology. This patient admitted to poor sleep (had trouble falling asleep and woke up often during the night), she suffered with moderate and occasionally severe anxiety, felt bloated and gassy after eating, had a chronic low back pain syndrome, and stated that in addition to the foot pain she was suffering, her feet were always cold (sometimes painfully cold). She also stated that she only drank 1-3 glasses of water daily. Right off the bat, these are signs that this patient has problems that could very well affect the efficiency of the immune system. Poor sleep is a big one because it is during sleep that the body works to maintain homeostasis by repairing injured cells, replacing dead cells, detoxifying all of the cells in the body and replenishing what has been used up (e.g. hormones, enzymes, neurotransmitters, immune cytokines, carrier molecules, etc.). Someone who does not sleep well often has a very difficult time healing compared to the general population. Anxiety is often caused by elevations in adrenal hormones and/or imbalances in inhibitory and excitatory neurotransmitters (the chemical messengers of the nervous system). Both of these issues have direct inhibitory effects on the immune system and can make it very difficult for the repair and detoxification pathways to function properly. Couple this with the fact that the patient was taking anti-inflammatory medication which directly suppress the pathway of chronic inflammation causing her pain, but also inhibits the pathway of primary inflammation, which is the 4 arms of homeostasis - repair, detoxification replenishment and replacement.
The gas and bloating is another sign of possible impaired healing since most chronic GI symptoms have a direct relationship to immune activity (since ¾ of the immune system is found in the GI tract). Her chronic low back pain may be coming from the same cause as her foot pathology or it might be influencing the way she walks and hence putting more stress on her foot and is an important part of this functional medicine differential diagnosis. Her cold feet (known as Raynaud’s Disease) is a critically important finding for foot pathology, especially since connective tissue has no direct arterial blood flow. These tissues are fed by microscopically small capillaries. Raynaud’s Disease is a syndrome where these microscopic capillaries go into spasm, essentially reducing blood flow to the inflamed and injured tissues. Without adequate blood flow, nothing can heal. Finally, inadequate water consumption is a huge factor in healing since almost all chemical reactions in the body require water.
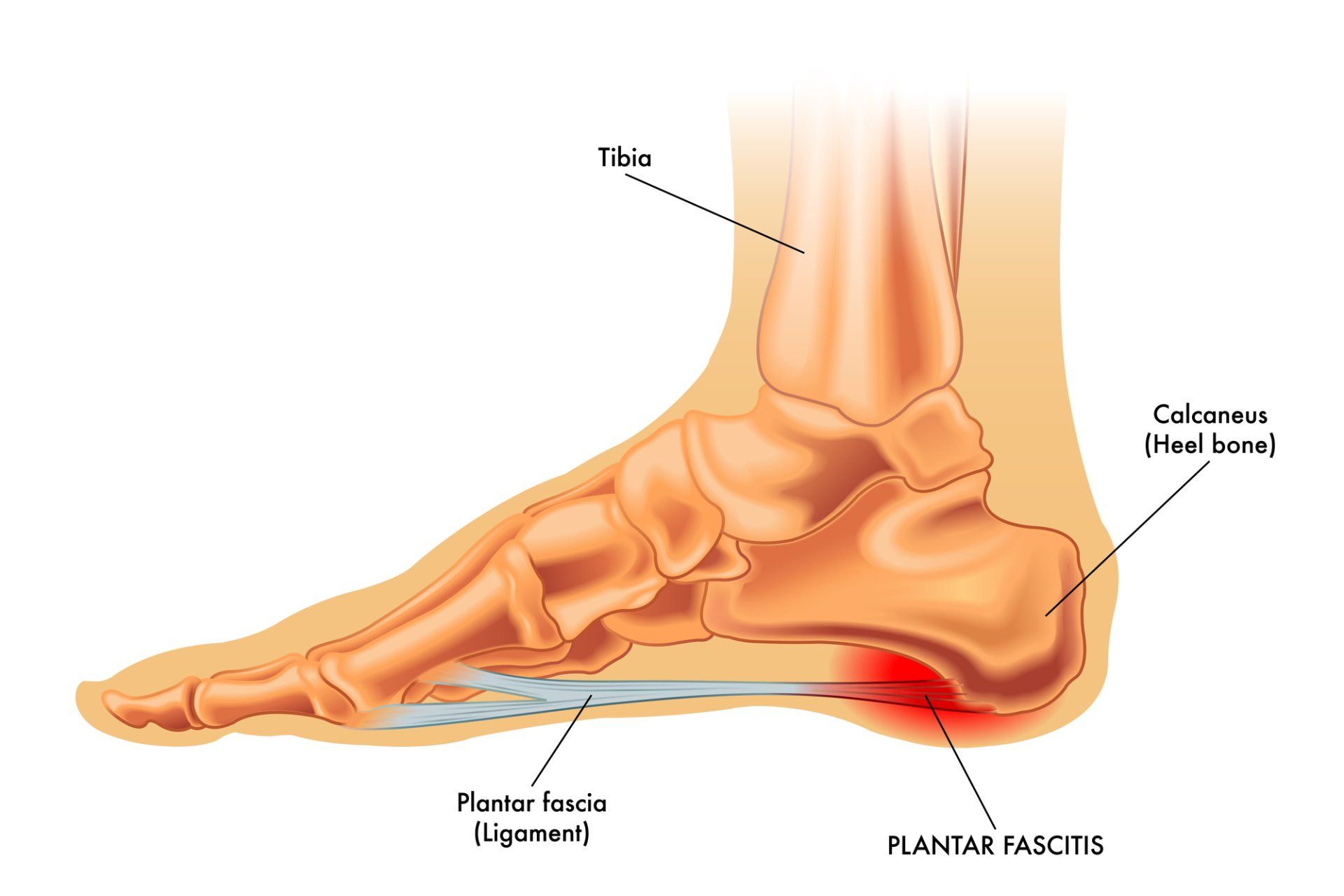
So, without even examining her foot, I was already seeing numerous reasons for her inability to respond to conventional therapy. The examination revealed a biomechanical issue called functional hallux limitus, which is a condition that usually worsens with an arch support type of orthotic (exactly what her first podiatrist gave her). A sonogram revealed inflammation and a small partial tear of her plantar fascia (the arch supporting ligament), which in all likelihood was caused by the steroid injections. Steroids are fibrolytic and are known to weaken ligaments and tendons. They are much more likely to cause this in patients with poor microscopic blood flow since they are unable to detoxify and remove the steroid that was injected into the area in a timely way, hence increasing the time it has to weaken the ligament. This is why her pain levels began to increase in spite of “treatment”. The heel spur had nothing to do with her pain. The spur is a symptom of extraordinary stresses on the plantar fascia which was obviously inflamed and the cause of her original pain.
Sleep disturbances, anxiety and Raynaud’s are all often due to adrenal/neurotransmitter issues, so I prescribed an adrenal stress test (saliva samples) and a neurotransmitter assay (urine sample). We also find that stress hormones or an excitatory neurotransmitter dominance can cause slow digestion as these hormones are designed to slow metabolism to preserve energy during times of stress. She had shared all of these symptoms with her internist who prescribed an SSRI called Xanax for her anxiety and Ambien for her sleep. She did not feel well taking the Xanax and did not like waking up groggy from the Ambien so had not really used these medications in quite some time. In addition, stretching only one muscle group (the calf muscles) can cause more functional imbalances since the muscles of the lower extremity are synergistic. A full lower extremity stretching regimen was prescribed to her to increase flexibility, assist with filling the muscles with more blood and facilitating release and elimination of built-up toxins in the muscles. She was also instructed to increase her water intake by one glass/day/week so that by the end of 6 weeks, she would be consuming about 8 glasses of water a day. Water is introduced slowly since the body is compensated to function without it. That is why people who don’t drink enough water are not often thirsty. Too much too soon just sends the patients scrambling to find bathrooms all day. Once the body begins to use the water, then these patients report that they are now experiencing thirst throughout the day.
The lab results revealed serious elevations in her cortisol levels as well as elevations in two excitatory neurotransmitters, Glutamate (the primary excitatory neurotransmitter) and Epinephrine (which is responsible in many patients for peripheral microscopic vasospasm). It is postulated that these imbalances cause anxiety and sleep problems. However, it is also entirely possible that chronic anxiety and sleeplessness causes changes in adrenal and neurotransmitter behavior. These changes are part of a primitive survival mechanism and are activated in times of danger. For example, our long-ago ancestors had to fear being eaten by animals. When presented with this danger, the adrenals release cortisol which is a hormone designed to extract sugar out of our cells and deposit it into the bloodstream where it can be quickly pumped to the muscles used for defense (either the arms to punch and protect or the legs to run away). They are quickly pumped as the epinephrine does two things. First, it speeds up the heart rate and second, it steals blood from the extremities to be able to pump larger amounts of blood to the arms and legs (thereby producing cold hands and feet). This is commonly known as the fright, fight and flight response.
In modern life, we are bombarded by stress in the form of family issues, war, murder, crimes against our homes, TV news, politics, noise, financial stress, drugs, etc. This chronic form of stress mimics what happens when our ancestors were able to escape the beast and hide in the bushes. Once safe in the bushes, they had to stay put until the beast left the area. This meant that they couldn’t go feed themselves since leaving their hiding place in the bushes made them vulnerable to attack. Physiologic changes must be induced by stress hormones, one of which is to suppress thyroid function and slow the basal metabolic rate. This preserves calories and energy while the person is unable to go find food. In addition, sleep becomes dangerous because in deeper levels of therapeutic sleep, you would not hear the beast sneaking up on you. So sleep cycles must change. Lighter sleep is a hallmark of this syndrome. Finally, because there is no food coming in, digestive enzyme secretions begin to diminish, thus preserving the enormous amount of energy expenditure required for digestion. But if this is a person from today, they will continue to eat and suffer from slow digestion leading to all kinds of varied GI symptoms.
For this patient, the adrenal/neurotransmitter was addressed with Targeted Amino Acid Therapy. This is a completely natural approach to correcting this, thereby increasing blood flow in the foot and coincidentally improving her sleep disorder, reducing her anxiety and GI symptoms. Once she reported improvement in these symptoms and I knew the immune system was more efficient now, we began a course of prolotherapy which is a non-surgical, non-steroidal injection technique that fortifies and strengthens ligaments and tendons and we were able to get the plantar fascia to heal. In addition, instead of the arch support, I made her a torsional foot orthotic which addresses the biomechanical problem more efficiently. Ultimately, this patient who suffered with chronic foot pain was able to heal and at the same time, have her overall health improve. This is the goal of functional medicine. We address the causes of the problem, the reason it is chronic by discovering burdens on the immune system and then correct them.
For more information on this approach to chronic pain, you can go to drrobertkornfeld.com.
LONG ISLAND
Dr. Robert A. Kornfeld, DPM, Holistic Podiatrist
551 Port Washington Blvd. Port Washington, N.Y. 11050
(516) 369-3172
(516) 945-0888
MANHATTAN
Dr. Robert A. Kornfeld, DPM, Holistic Podiatrist
127 East 56th St. 4th Floor, New York, N.Y. 10022
(516) 369-3172
(516) 945-0888
All Rights Reserved | Chronic Foot Pain Center