HOW TO HEAL FROM CHRONIC FOOT PAIN
Take the Right Steps Toward Healing

The prevalence of chronic foot pain is on the rise. It is on the rise not just in the general population, but also in the population of foot sufferers who have already undergone traditional medical treatments. Many patients with chronic foot pain have been to numerous doctors. Some, more than 10 or 20 different doctors over the years. It is NOT that any of these doctors were poorly trained. It is that the paradigm of medicine we engage in in this country puts treatment first and assessment on the back burner.
By this, I mean that doctors typically make a diagnosis and then institute treatment. There is little to nothing done in the way of trying to find the mechanisms (the reasons) that explain why this patient suffers from chronic pain and has failed all attempts at trying to get the pain to resolve. As a doctor who specializes in chronic foot pain, I have treated thousands of patients over the years who come with a long history of failed treatments. This population of patients needs deeper assessments. Not just a diagnosis and therapies that attempt to suppress pain and inflammation. But assessments that begin to explain why this patient continues to suffer in spite of everything already done. Treating pain in any way without understanding underlying causes is like chasing a speeding train.
It starts with an understanding of how the human body is designed to maintain optimal health. We have endogenous (built-in) pathways that work to detoxify our cells, repair injured tissues, replace dead cells and replenish what is used up (i.e. enzymes, hormones, neurotransmitters, cytokines, carrier molecules, etc.). When these different pathways are functioning optimally, then the body can achieve homeostasis (efficient function and optimal health). In order for these pathways to function optimally, it is essential that the body has a proper supply of necessary nutrients, vitamins, minerals, proteins, fats, water etc. It is also critically important to the success of these pathways that there is adequate sleep. For it is when we sleep that the majority of work to achieve homeostasis is accomplished.
Therefore, a patient in chronic pain needs more than a diagnosis. They need a complete epigenetic assessment (of diet, lifestyle and environmental factors) and how that alone might burden the immune system and create struggles physiologically. In addition, lab assessments that can identify inefficiencies in any of the arms of homeostasis need to be done. For example, one of the most common burdens on the immune system in addition to poor diet, sedentary lifestyle and poor sleep habits is poorly managed stress. The stress response is controlled by adrenal hormones and neurotransmitters and is a primitive survival mechanism. Chronic stress causes adrenal or neurotransmitter imbalance which directly burdens the immune system making it difficult to digest and assimilate food, interfering with healthy sleep cycles, suppressing thyroid function and slowing down the basal metabolic rate (making it difficult for the immune system to keep up with the typical challenges of everyday living). Looking at lab evaluations of adrenal circadian rhythms as well as neurotransmitters can help shed light on many of the mechanisms making for a chronic pain experience and can be treated without drugs.
We can also assess the pathways of detoxification; of nutrient balance and supply; of sensitivities to foods that ramp up inflammation; of the types of circulating fatty acids (some of which when dominant feed the pathway of chronic inflammation); of gut health (the friendly bacteria in your gut are responsible for a fermentation process that gives rise to the short chain fatty acids that feed your immune system) and many others so we can get a better understanding of each patient’s unique physiology and ultimately see where we need to intervene to get these mechanisms under control (patient-specific assessment). This may include changes in diet, proper exercise regimens, nutrient supplementation, sleep hygiene, improved hydration, etc.
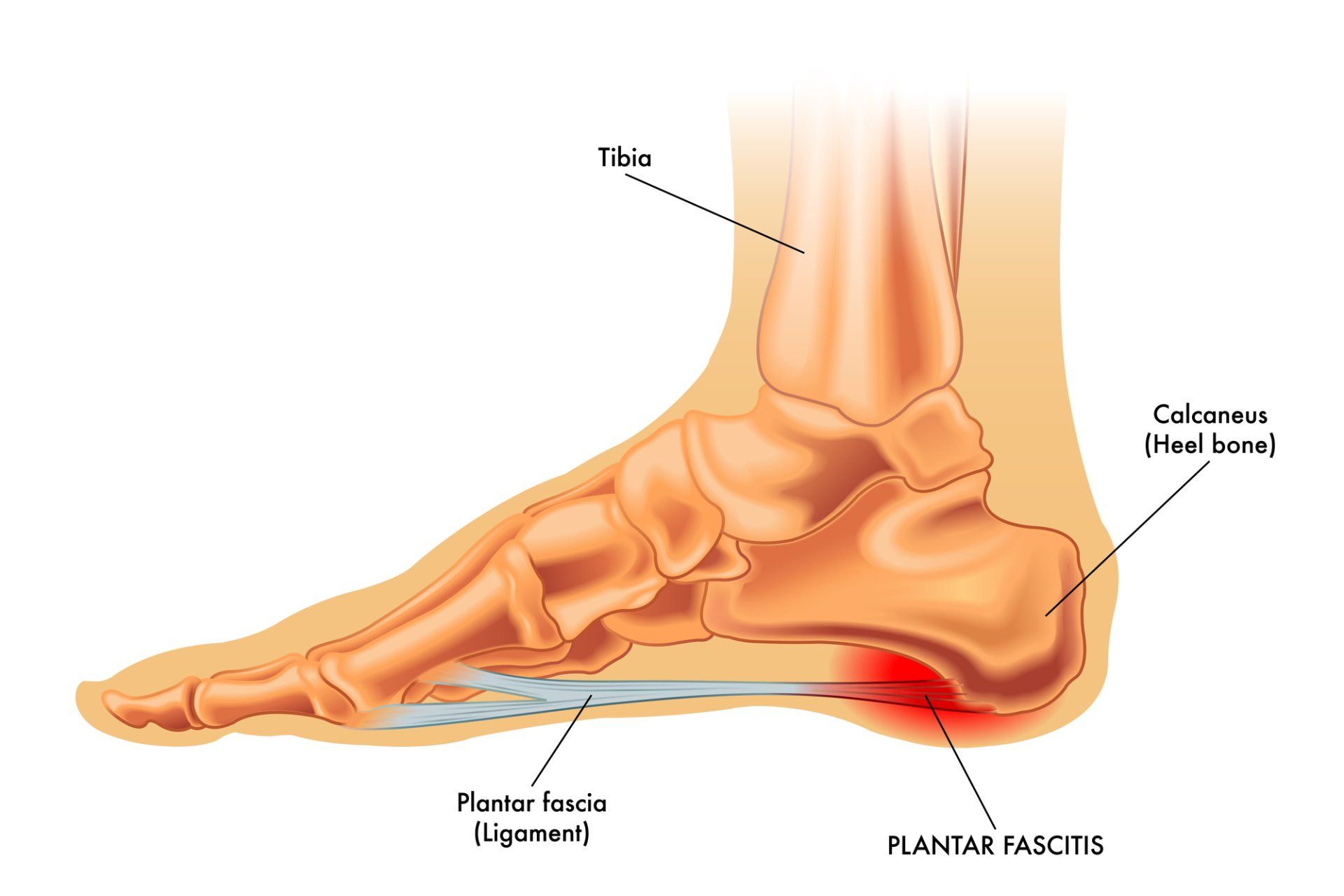
Once we have the physiologic mechanisms managed, then we look for other contributory mechanisms. When it comes to foot pain, one must assess the structure and function of the lower extremity. This approach, called biomechanics, can tell us how we need to control the aberrant biomechanics, thus minimizing the physiologic challenges placed on the foot and ankle. A proper physical therapy and foot orthotic approach would then be prescribed.
Finally, we institute therapies to support (rather than suppress) the body’s ability to detoxify and repair the cells that are struggling to heal. This is done through biologic response modification, meaning converting the chronic inflammation to primary inflammation (detox, repair, etc). This can be accomplished by increasing perfusion of blood into the foot and ankle with high voltage electrical stimulation (the human foot is the least perfused area of the body. Blood flow is the ultimate determinant of all healing); homeopathic injections (mild natural medicines that initiate the detox/repair pathway)), prolotherapy injections (medicines that gently disrupt cell membranes and foster the call to repair), platelet-rich plasma injections (utilizing the patient’s own platelets which are rich in growth factors that facilitate repair)or amniotic fluid allograft injections (containing stem cells and lubricants that heal and protect). All of the injection therapies foster repair in different ways. They do NOT suppress inflammation like cortisone. They actually help foster and facilitate repair and strengthening of the involved tissues. We do not need to field side-effects in the way we do when we are suppressing natural body function.
As you can see, it’s a step by step approach to ultimately not only resolve the pain syndrome, but to leave the patient in a much better state of health.
Dr. Robert Kornfeld is the founder of The Chronic Foot Pain Center with offices in Manhattan and Long Island. His 38 years of experience and his sub-specialty focus on the natural treatment of chronic foot pathology makes him uniquely qualified to assess and treat all kinds of chronic pain syndromes of the foot and ankle. To learn more, check out his website at www.drrobertkornfeld.com as well as his Facebook page at Chronic Foot Pain Center – Dr. Robert Kornfeld.