Accepting New Patients
Treating Achilles Tendon Injury and Inflammation
Treating Achilles Tendon Injury and Inflammation
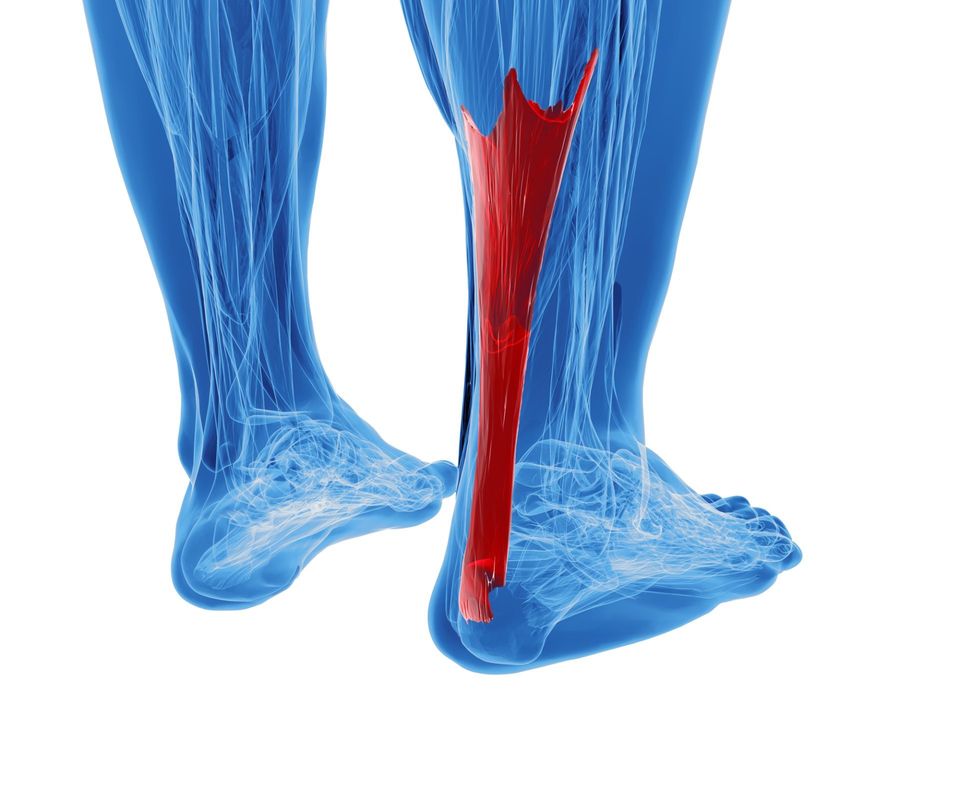
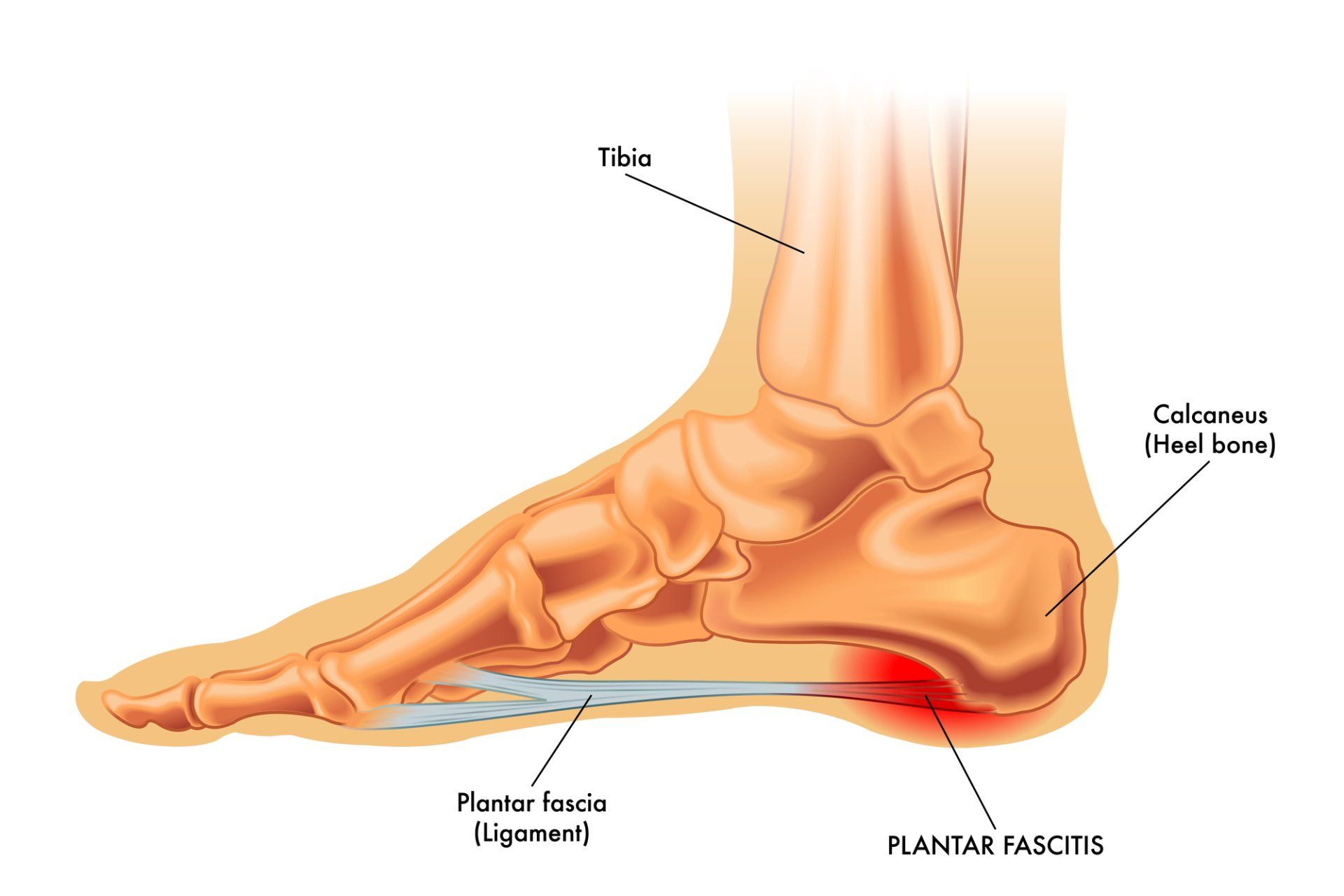
One of the more common, yet difficult conditions to treat is Achilles tendinitis. The Achilles tendon attaches the calf muscle to the heel. The role of the calf is to lift the heel off the ground. In order to do this, it must be strong enough to overcome gravity and the full weight of the body in order to lift the heel and propel body weight into the forefoot where the action of propulsion occurs. As such, it is the largest and strongest tendon in the body.
There are many different causes of Achilles tendon inflammation and because of the fact that this tendon is a workhorse, it can be very difficult to calm the inflammation and get the injured cells to heal. When the tendon is forced into a workload that is beyond its physiologic capabilities, cells in the tendon can be pulled and injured or even torn. Sometimes the tears are microscopic and continue to happen over time. Sometimes there are more traumatic and frank tendon tears or ruptures.
Sports and fitness enthusiasts (like runners) are more prone to frank tears and ruptures but also can develop microscopic tears that lead to chronic tendinitis. What is most important in assessing the cause of tendon injury is the level and type of activity as well as the type of training (stretching and strengthening). A thorough look at biomechanics is essential (structure and function of the lower extremity) to discover any functional reason why the tendon is under stress.
Non-athletes can, of course, also develop this condition from poor biomechanics. In addition, once injury has occurred, any immune burdens, circulatory disorders or nutritional deficiencies can impede healing. A comprehensive analysis is essential in treating this condition. We must identify the mechanism (cause) and anything that blocks healthy pathways of repair (diet, lifestyle, patient-specific physiology) and make those corrections. This may include temporarily immobilizing the tendon followed by functional foot orthotics, stretching and strengthening exercises, dietary changes, addressing immune burdens, and treating the cellular injury.
My preference for driving the repair of the cells is to utilize high voltage electrical stimulation which drives more blood into the tendon along with prolotherapy, which is an injection technique that fosters fibroblastic activity (the generation of new cells that convert to tendon tissue) thereby healing AND strengthening the tendon. Cortisone injections are not recommended in a tendon that has this level of physiologic load to deal with because cortisone is fibrolytic (thereby weakening the tendon) and can lead to doctor-induced tendon rupture.
Healing of this type of condition must be methodical and the patient must be patient with the process. There is no rapid magic bullet. Seeing it through will not only heal the tendon but make future injury far less likely. Also, when we address mechanisms of pathology along with supporting the pathways that facilitate repair, we wind up with a healthier patient than we started with. That, in my paradigm, is the most important result.
LONG ISLAND
Dr. Robert A. Kornfeld, DPM, Holistic Podiatrist
551 Port Washington Blvd. Port Washington, N.Y. 11050
(516) 369-3172
(516) 945-0888
MANHATTAN
Dr. Robert A. Kornfeld, DPM, Holistic Podiatrist
127 East 56th St. 4th Floor, New York, N.Y. 10022
(516) 369-3172
(516) 945-0888
All Rights Reserved | Chronic Foot Pain Center