Plantar Fasciitis: Overcoming Heel and Arch Pain Naturally
Plantar Fasciitis: Overcoming Heel and Arch Pain Naturally
Have you ever thought about the work your feet do every day? Those two small appendages at the bottom of your leg not only support a body which is comparatively massive in size but are also responsible for transporting that body approximately 2,000 miles per year. Your feet are the foundation of your physical form–literally the base on which you are built–but most people treat their feet as though they could unzip and detach them at the end of the day. We mindlessly abuse our feet until we are injured or in pain. Only then do we pay them their due respect.
Sadly, the prevalence of foot and ankle problems has skyrocketed over the past three decades. Millions of Americans suffer from foot and ankle injuries every year, and many people are experiencing these disorders at a much younger age than a generation ago. I’m sure many of you reading this are part of those statistics.
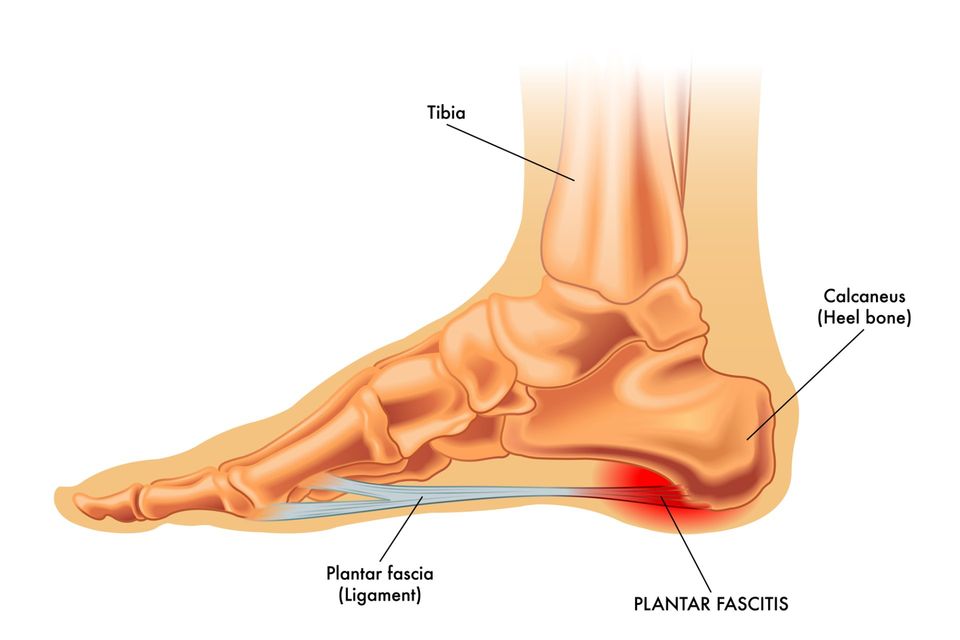
One of the most common foot maladies people suffer from is plantar fasciitis. This condition arises when undue stress is placed on the ligament in your foot that supports your arch–the “plantar fascia”. When that ligament is overworked it leads to the classic symptoms of heel and arch pain which worsens when you get up to walk after periods of rest.
Understand that this isn’t the kind of pain you experience after being on your feet all day at work or walking around Disneyland with your kids. The pain from plantar fasciitis is often intense and debilitating. It is also surprisingly common. Two million Americans suffer from plantar fasciitis every year and 10 percent of the population will experience it in their lifetime. It has become recognized as one of the most chronic and, often times, most difficult foot problems to treat.
Perhaps this is because few podiatrists take an integrative approach to foot problems like plantar fasciitis. Like most people, doctors typically think of the foot as somehow separate from the rest of the body–they focus on treating only the foot and don’t look at the other physiological systems or diet and lifestyle factors that go into creating these problems in the first place.
But your foot is connected to the rest of your body. If you want to heal a chronic foot problem, you need to treat your whole body. I have had immense success treating plantar fasciitis and other difficult-to-heal foot and ankle ailments in my practice using this kind of integrated approach. Understanding the concepts in this article is critically important if you are to heal your feet and put an end to the pain and debilitation of plantar fasciitis.
Inflammation: The Pathway to Foot Health and Illness
When your plantar fascia is stressed–whether you are beating it up with improper exercise, have a congenitally short ligament (which causes a “cavus deformity” or extremely high arch), or your calf muscle complex is too tight and thus pulling it in the opposite direction–the cells in the ligament become more metabolically active and cellular damage occurs.
When this happens, the immune system is recruited to help detoxify the cells and repair the injured and damaged ones. It does this via a cascading pathway known as primary inflammation. When this pathway is operating efficiently and it is able to properly handle the extent of the injury, you will have no symptoms or they will be minor. You may experience some slight pain and swelling in the area that has been affected. This will diminish rapidly (within a few days) as your injured ligament is repaired.
When the stress you have placed on your foot is greater than this pathway can manage, your immune system employs a different set of chemical responses and a different pathway is activated. That pathway is chronic inflammation.
Chronic inflammation is designed to protect your tissues when they are under extreme stress in the hopes of preventing permanent damage to your system. The problem with chronic inflammation is that when it is left unchecked it actually creates further damage and produces profound pain, swelling, heat, and other symptoms. This is usually when people wake up to their feet–when they are hobbling into my office.
The impact that inflammation has on the body is one of the most profound discoveries in modern medicine. Chronic inflammation can contribute to a host of chronic illnesses from heart disease, to diabetes, and more. It is also the driving force in plantar fasciitis.
But what’s most extraordinary about inflammation is that it can either heal your body or make you chronically ill. It just depends on which pathway is activated. In the case of foot disorders, primary inflammation is a powerful healer. So, my job as a holistic podiatrist is to stimulate the pathway to healing (primary inflammation) and block the pathway to plantar fasciitis and other forms of foot pain (chronic inflammation). We need to utilize the body’s inherent ability to detoxify and repair the cells that have been injured, while at the same time eliminating the possibility for further injury.
Understanding inflammation this way is a fundamental shift away from the way most conventional podiatrists understand and treat plantar fasciitis. The most common treatment for the condition is cortisone, a powerful steroid that blocks inflammation. The problem with cortisone is that it blocks ALL inflammation. Sure, it relieves the immediate symptoms of the problem. But it ultimately inhibits the body’s inherent mechanisms for healing itself.
This is further complicated by the fact that cortisone is “fibrolytic,” which means it can weaken fibrous tissue. All connective tissue–tendons, ligaments and joint tissue–is fibrous tissue. Your plantar fascia is fibrous tissue. So it’s not a great idea to take medications that weaken this tissue when you are looking to heal and strengthen your ligaments.
Put simply, cortisone cannot be relied on as an effective treatment. However, there are ways you can properly support the pathway to healing and overcome plantar fasciitis. Here’s how you do it.
Treating Your Feet from the Ground Up: Diet/Lifestyle Changes to Heal Plantar Fascitiis
There are two factors we need to consider when treating plantar fasciitis. The first are the “functional influences” on the foot–that is, the mechanics of how you use your foot and how that influences its health. The second is identifying burdens on the immune system that make primary inflammation less efficient.
There are many reasons the plantar fascia can become painful and inflamed. Common problems that contribute to the condition are:
- Structural deformities
- Repetitive stress injury
- Muscular dysfunction
- Positional deformities
- Abnormal muscle sequencing
- Improper or excessive exercise
- Secondary muscular compensations
You need to identify and address which of these issues is leading to problems with your plantar fascia. The treatment will depend on exactly what you are doing to injure your foot. For example, if you are exercising improperly you can learn better technique. Additional common interventions include:
- Stretching exercises
- Therapeutic exercises
- Orthotic therapy (extremely important if needed)
- Yoga
- Physical therapy
The goal is to correct these biomechanical problems to the degree possible. Once this is accomplished, we can focus on healing the inflamed and injured tissue without fear of continued stress and injury. That is where the second factor in treatment–metabolic influences–comes into the picture.
Remember, to heal your feet you need to heal your whole body. Supporting the pathway of primary inflammation means looking at the dietary, lifestyle, and environmental influences that positively and negatively affect it. Put another way, we need to make sure you are giving your body what it needs to heal itself.
Since all injured tissue (including your plantar fascia) requires oxygen and nutrients for healing, the first place to look for any nutrient deficiencies is in the diet. Here is what I recommend you do.
For one week, journal about your current diet. Take careful notes on everything you eat and drink. Don’t just try and keep track of this in your head. Write it down. This will give you a much better sense of what you are eating every day. Then you can assess if there are any ways you can optimize your diet. Do you eat too many refined carbs? If so, cut them out. Do you consume too much or the wrong kinds of protein? If so, cut back or focus on healthy proteins full of omega-3 fats like small wild fish, nuts, and seeds. Are you eating enough vegetables? If not, up your intake. You should be getting at least 5-9 servings a day.
In addition to optimizing your diet, I often recommend the following nutritional supplements to assist in the healing process:
- Omega 3 fatty acids (from fish oil) – These help regulate the inflammatory process and support the pathway of primary inflammation.
- Amino acids – The building blocks of all connective tissue are a base requirement for cellular repair processes.
- Anti-oxidants – Prevent the buildup of free radical compounds in the area of chronic inflammation by taking these in supplement form and you will ward off degenerative changes in your tissues.
- MSM – A form of dietary sulfur, this powerful supplement aids in the healing of inflamed connective tissue and helps strengthen those tissues.
- Probiotics – These healthy gut bacteria are needed for the production of short chain fatty acids which literally feed your immune system and make all immune related activities more efficient, thereby reducing inflammatory pain.
- Curcumin – This extract from turmeric, is a biological response modifier and bolsters primary inflammatory efficiency. It is a powerful anti-inflammatory.
- Hydration - You will also likely need to increase your water consumption. Water is the essential environment for all metabolic processes in the body. Proper hydration facilitates cellular repair, and most people don’t get enough water. You should drink a minimum of eight 8-ounce glasses of water every day.
If you still have problems after taking these steps, the next thing you need to do is identify potential immune system challenges–factors that make your immune response less efficient than desired. This usually involves some laboratory work. Here are some of the tests I typically perform to help tease out these kinds of problems:
- Food sensitivity tests – These tests are done to uncover the possibility of foods that are “irritating” to the immune system. These are not allergy tests. They are done to identify foods, which may be misdirecting the immune system and increasing inflammation in your body. Finding out which foods you are sensitive to and eliminating them from your diet will free your immune system to perform its regular duties more efficiently. I often see great improvement in healing stubborn conditions like plantar fasciitis by treating food sensitivities.
- Lipid peroxide assay – This test will reveal whether or not your body is properly controlling the rate of formation or elimination of free radical compounds in your body. High levels of free radicals also serve to misdirect the immune system by triggering genes that lead to degenerative diseases, such as arthritis. What does this have to do with inflammation? Well, these genes are “turned on” by the chronic inflammatory pathway–the very same pathway that leads to plantar fasciitis and the debilitating pain it causes.
- Fatty acid RBC assay – This is a comprehensive test designed to identify all of the fatty acids inside your red blood cells. The test does not determine what kinds of fatty acids are being absorbed into the bloodstream, but rather quantifies the levels of all fatty acids being utilized by each of your cells. This is important because fatty acids determine the type and efficiency of inflammation in your body.
- Adrenal stress hormones – This is an important test to perform in individuals battling chronic pain. Stress hormones are nature’s protection against stressful life events. They help us adapt in life threatening situations by triggering the “fight or flight response”. But when we are running from danger or protecting ourselves against danger, the body turns all its energy to the task at hand and forgets about repairing injured cells, digesting foods, and other important activities needed for healing. When your stress hormones are out of balance and chronically activated, it becomes very difficult for your immune system to function optimally. That means you heal more slowly and your plantar fasciitis does not resolve as readily.
In some cases, it is also necessary to treat local inflammation aggressively when you have plantar fasciitis. But, cortisone is not my favorite medication for dealing with this condition. So when people are in extreme pain and need immediate relief, how do we help them?
We still want to foster primary inflammation, and I have found homeopathic injections extremely helpful in facilitating the healing of inflamed tissue in a localized way. Homeopathic injections stimulate your body to detoxify and repair cells in the area they are injected with absolutely no worry of further damaging your tissues the way cortisone can. Here is how it works.
Upon injection, homeopathic molecules bind to the tissue in the area they are injected into–in this case the inflamed plantar fascia. The immune system then reads that there is something there that shouldn’t be, and enables a primary inflammatory response to detoxify the tissues–the very response you want to encourage to heal plantar fasciitis. The beauty of this is that you get immediate temporary relief from pain while stimulating your body to heal itself at the same time. With continued treatment, the pain intensity and frequency begin to wane until healed. It’s a win-win treatment.
The reason plantar fasciitis is considered so difficult to treat is because the medications conventional medicine uses do not address the cause of the problem. The key is to identify and address issues in the whole body that are either directly or indirectly impacting the plantar fascia. Once you have done that you have a much better chance for healing than simply taking injections of cortisone or anti-inflammatories. These medications do not optimize health in any way, shape, or form, and they certainly don’t treat the cause of your foot problems.
I have been treating patients who come to see me with plantar fasciitis using the steps above for over 30 years. I have never seen any negative reactions, and most people get completely well. An occasional patient does not respond completely and then, of course, there are more aggressive therapies that I may employ.
You can take most of these steps on your own. Others you can work through with a practitioner of integrative medicine. But what you want to do is focus on treating the cause of your foot pain, not mask your symptoms with medications that may actually make the problem worse.
And who knows? You may see an improvement in other areas of your life as well. Every one of the steps in this article is part of a larger path toward improved health–not only for your feet but for your whole body. That, in my opinion, should be the goal of every doctor and patient in this country.
Remember, your feet are connected to the rest of your body. They may be way down there at the end of your legs, but they are no less a part of you than your brain or heart or lungs are. Take care of them and they will take you wherever you wish to go for many years.