Maintaining Lower Extremity Sports Health After Injury
Getting Back to An Active Lifestyle

There is no question that this era has birthed an explosion in the areas of fitness and nutrition. Unlike past generations, baby boomers and their children are more active, more fit and more concerned with their overall health than generations past. This is a wonderful thing. Studies show that keeping physically fit and eating well improves health and longevity across the board.
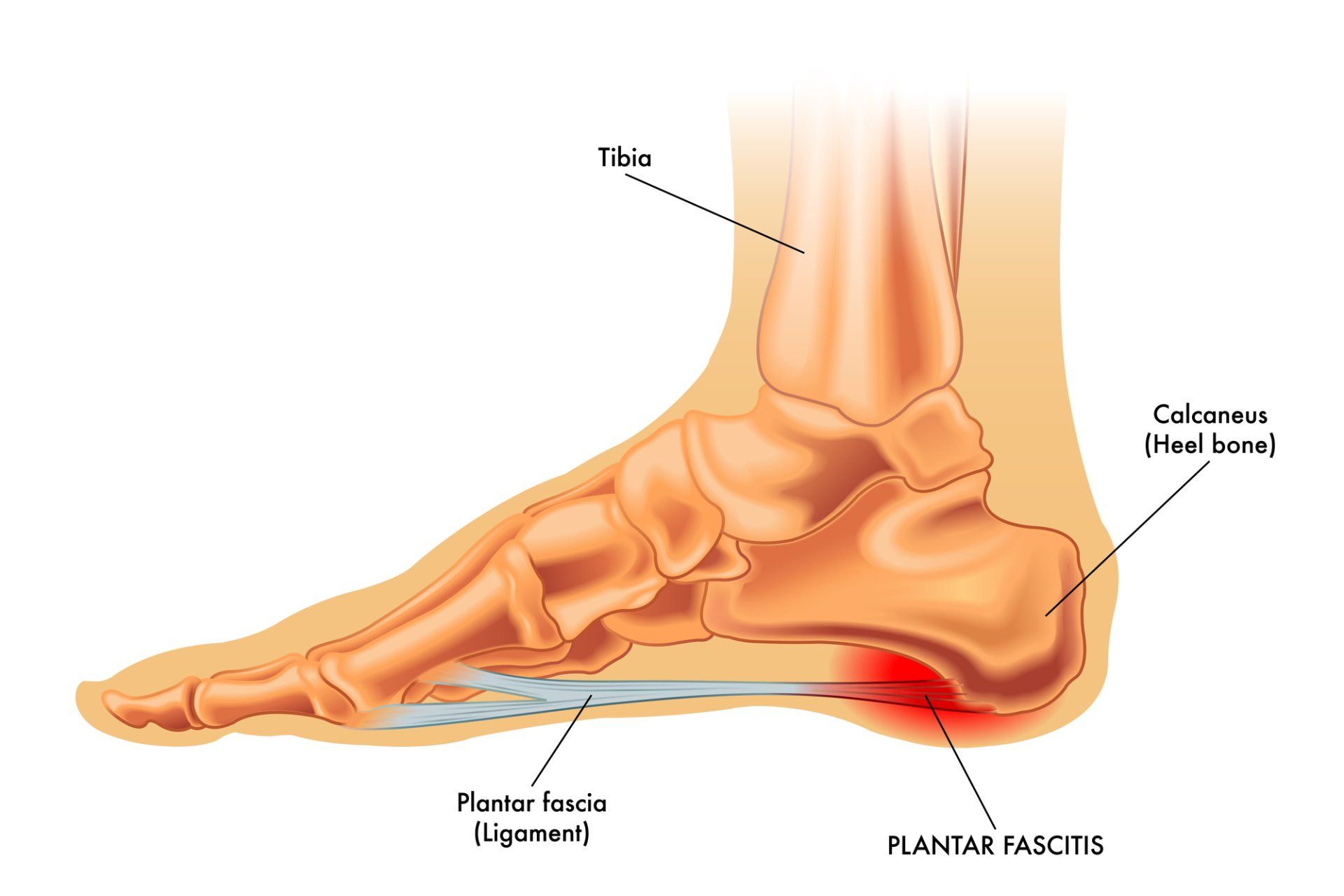
If you walk into any gym or fitness club in America, you will undoubtedly see treadmills, elliptical machines, stair climbers, stationery bikes and spin bikes for cardio conditioning and weight management as well as weight stations and free weights for strength building. All of these different methods of working out (other than upper body weight training) depend on the lower extremities for results. That is, the foot, the ankle and the legs are the keystone of all of these endeavors. It is no wonder, then, that many well-intentioned people wind up developing pain syndromes and injuries of the foot and ankle. As a foot and ankle specialist for more than 35 years (with a concentration on chronic pain), I have seen thousands of these patients over the years for treatment.
When treating injuries, we must keep TWO things in mind. The first of course is healing the presenting injury or syndrome. The second is making sure that we ultimately decrease the chances of this happening to the patient again. And this is something that seems to not always be accomplished by the traditional approach to medical care. Allow me to clarify.
Pain syndromes (other than direct injury) develop from repetitive stress on tissues that are unable to withstand those stresses and wind up getting injured. Injured tissues are managed in the human body by a pathway called primary inflammation which fosters the detoxification and repair of these injured cells. However, when cells cannot heal readily and the stresses continue, the pathway is then changed. Instead of trying to repair tissues, the immune system will opt to protect what it cannot readily heal. This pathway, called chronic inflammation, is responsible for the pain you feel when your foot or ankle is hurting and seems to not want to heal.
The great majority of patients who seek medical care for these problems will meet with a doctor and are offered anti-inflammatory therapy, either via a cortisone injection or a non-steroidal anti-inflammatory medication. Both of these approaches will provide relief, but not without some risk. Cortisone is an anti-inflammatory medication and can relieve pain from chronic inflammation but it is also fibrolytic, which means it can weaken or damage connective tissue (tendons, ligaments and joint capsules). In safeguarding our patients’ future sports performance, taking this risk may not always be a good idea. Some patients are left prone to further injury because the involved tissues are now weaker than before and will not be able to handle the stresses placed on them again. Other patients go on to tendon ruptures. The other option, non-steroidal anti-inflammatory drugs (NSAIDS), should also be well understood. NSAIDS also suppress inflammation and therefore can provide relief. Unfortunately, they not only suppress chronic inflammation, they also interfere with the pathways of detoxification and repair. Patients on NSAIDS need to have their livers monitored due to the fact that detoxification is impaired while on the drug. As well, the healing of the involved tissue may, in certain patients, be incomplete because of the pharmaceutical blockade. This means that not only will the pain return when the drug is withdrawn, but further damage may have occurred during the time that the pain was suppressed and the foot or ankle was still being used and put under stress.
In my opinion, neither of these remedies makes sense in the BIG picture. I understand that patients want to be out of pain, but my job as a doctor is to heal the problem and safeguard their future sports health so that once better, they can return to their fitness endeavors with a far lower incidence of recurrent pain.
To accomplish this, we need to understand how the human body works and support the pathways that foster the repair and strengthening of the involved tissues. This means ensuring that the nutritional precursors to cellular repair are provided in the diet or by supplementation; that the patient sleeps well (the majority of healing and repair is accomplished during sleep); that they are well hydrated; that there are no current burdens on the immune system (be it elevated stress hormones, neurotransmitter imbalances, poor diet, etc) and that the therapies employed for healing have no deleterious effects on the injured tissues or their overall health. All immune burdens need to be addressed. This not only frees the body to heal better, but improves the patient’s overall health. This could include dietary changes, sleep hygiene, nutritional supplements and stress management.
Once accomplished, we can direct treatment at the involved tissues. My preference has been to utilize homeopathic injections (which I have been using for over 30 years with no negative reactions). These medicines foster the detoxification of the inflamed cells by removing inflammatory infiltrates and help to stimulate the natural pathways of tissue repair. They are not fibrolytic. They do not weaken tissues. Another direct healing approach is prolotherapy injections which also do the same thing but not quite as gently as homeopathic medicines. They are designed to create a bigger push toward healing but can cause some temporary increase in inflammatory pain after the injection is delivered. Prolotherapy is much better at strengthening the involved tissues and I use it when there seems to be some resistance to healing. Lastly, for the most difficult cases, I will use PRP (platelet-rich-plasma) injections. These injections utilize the patient’s own platelets which contain large amounts of growth factors needed to stimulate healing and repair. All three of these therapies are very successful when used in conjunction with all of the aforementioned immune support.
And, as always, when foot and ankle injuries are involved, we must look at any structural or functional imbalances that were part of the etiology of the problem. Functional custom-made foot orthotics, muscle strengthening (sometimes through high voltage electrical stimulation), stretching routines and physical therapy may be used.
Ultimately, we work toward facilitating a long sports/fitness experience for our patients. Focusing on the symptoms alone and not on the future lower extremity health is not, in my opinion, optimal medical care.
If you are experiencing a pain syndrome, foot specialist and podiatrist Dr. Robert A. Kornfeld of the Chronic Foot Pain Center in Manhattan can help. He has nearly 40 years of experience treating all types of foot-related issues, including all chronic foot and ankle pain, sports injuries, plantar fasciitis, achilles tendinitis, and torn ligaments. Call (516) 369-3172 to schedule an appointment or visit his website (www.drrobertkornfeld.com) to learn more about his therapeutic approach to relieve burdens on the immune system, improve local circulation to the foot, and enhance the body’s ability to foster homeostasis and healing.